Wednesday I met with the Long-COVID Clinic Neurologist for the first time, then yesterday I met with my speech/cognitive therapist (S/CT).
Neuro Takeaways:
At my age, with my Sx profile,1 and with what data they’ve been able to collect over two years, his general prognosis is that it will take 1 year for me to see something that looks like “stable” improvement and will be another 6–12 months after that before I feel fully recovered.
How do I feel about this? (a) it’s nice to have something remotely like a reasonable expectation about all this, (b) it’s nice to think that there will be an end date, (c) that’s a really freaking long time for a noob to hear!
Very much like ME/CFS, the important bit is to figure out your baseline of acceptable activity—physical and cognitive—that allows you to live day-by-day without crashing,2 then stay there. Maintain that baseline for what feels like a ridiculous number of weeks/months, then start adding tiny bits of activities back into the day—one tiny bit at a time, hold there, then, like a week later, add another tiny bit.3
The Data he’s seeing indicates that recently-acquired Long-COVID is not causing structural neurological damage (amen) but that it seems to be more signaling misfires or (a ha!) dysregulation—and signaling can be improved. So, I’m back to Jill Bolte Taylor: my next year will be spent working to get out of old neural grooves & building new neural pathways.
I asked about inflammation—about Parvo Virus causing neurological inflammation, narcolepsy potentially being caused by a version of the avian flu virus which also caused inflammation, my continuing5 adventures with gastro-inflammation. Specifically, I asked him if taking OTC anti-inflammatories prophylactically was worthwhile.
The gist I got from him was a big “meh”.
I also asked about taking half of a baby aspirin in the morning for similar reasons. “It probably won’t hurt you,” was not a ringing endorsement. However, he did say that baby aspirin isn’t a simple placebo—it’s “actually a pretty powerful blood thinner.” Duly noted.
He also mentioned—I managed not to laugh out loud—that it seems to be “inflammation dysregulation”6 rather than total and/or targeted systemic inflammation.
I need to see a PT for “Post-COVID Vestibular Rehab”—so that’s new. Has anyone else experienced something like this? Any idea what to expect?
I was impressed to see how he had me do the usual Neuro tests via a Teledoc call—he didn’t miss anything, that’s for sure.
I need to get blood labs taken for B-12. He said there’s been some data filtering in7 indicating that they’re seeing low B-12 across LC patients.
I asked if I should go get some sublingual B-12 or talk to my doctor about getting a B-12 shot after the blood draw. Apparently, it wouldn’t hurt, but I couldn’t tell if he thought OTC B-12 would or would not be enough to fill in the gaps the data is showing. More on that as I learn it.
Speech Therapy Takeaways
We have a new Long-COVID-specific APP! (And this one is being used for research, too!) VISIBLE! This thing is so new it’s still shiny! Right now it’s a pretty simple tracker with links to some reference materials. What’s really interesting is that they’re focusing directly on ME/CFS, Long-COVID, and “any other condition that requires the use of pacing.”
This will make sure you know where your
towelspoon is.
In pursuit of spoonish clarity, we reviewed the following:
Fog—when is it bad, what are the factors?
Most of my mornings are foggy—but they’re also largely silent. I only get anxious about the Fog if I (a) notice that three hours just evaporated, or (b) have to communicate with the outside world.8 This indicated to my S/CT that environmental triggers have a bigger impact on me and I’ll need to factor that into my spoon planning. If I know I’m going to be in a social situation—even briefly—I need to have a plan.
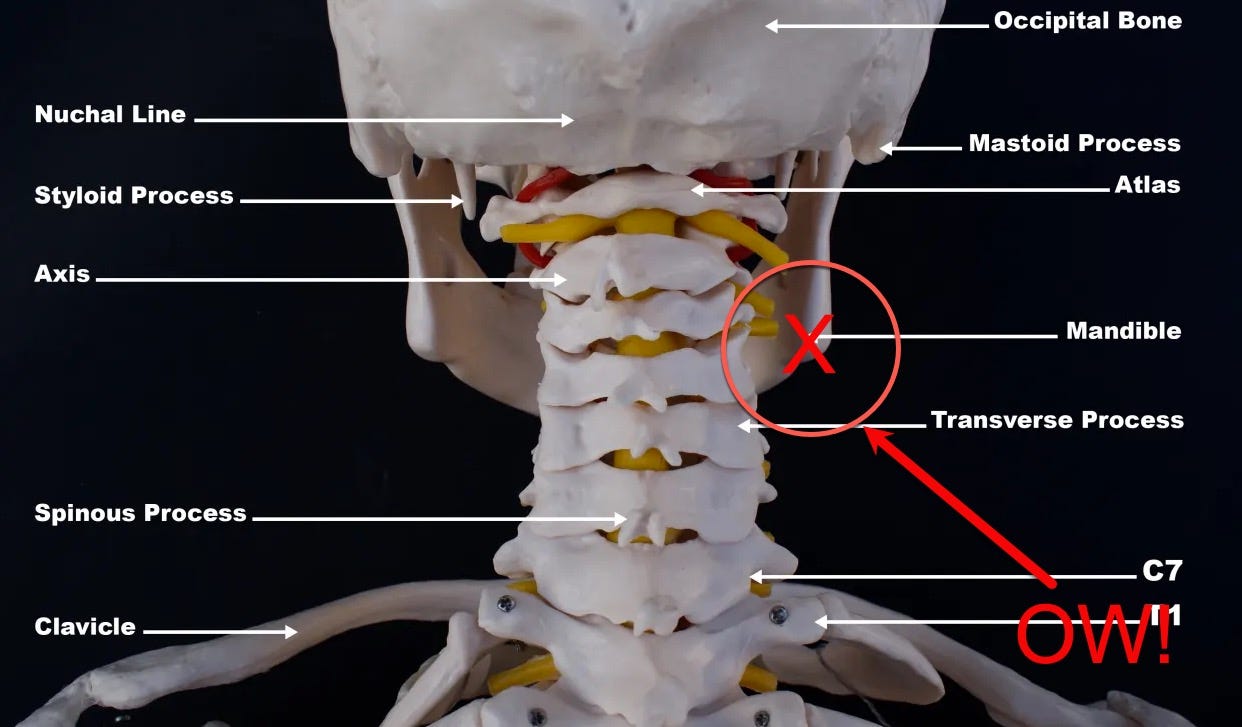
For example, at a not-long brunch last weekend, on Wednesday’s call with the Neuro, and on Friday with the S/CT, at around the 45-minute mark I got a sharp, stabbing pain in the back, right side of my neck (~an inch to the right of my C3/C4). Like a darning needle9 was stabbed in there, then removed. The pain shoots forward and then it’s all gone… until the headache starts about 15 minutes later.
So, now I know I have a “tell”—which I think is pretty useful in trying to learn my baseline!
What gives me the most anxiety?
Answering questions that require me to process and then make a decision in the moment. I mean, ridiculous things like, “Are you hungry?”—especially if I was doing anything else with my brain prior to the question—expose me as the utter mental void I have become.
S/CT recommendation: Ask for people to offer two categories (Chinese or Italian?) or two choices (eat at 6:30 or 7:30?).10
The thinking here is that—unlike the reasons why small children need simple, limited choices—for me it’s more of the need for a kick-start. I’m as likely to respond “Indian” or “8:00” rather than one of the given options. The idea is to get my brain aimed down the right track. I found that fascinating.
I’m also wondering if this isn’t simply a “good communication skill” when talking to someone with general anxiety.
S/CT also noted that pressure clouds thinking in general with Long-COIVD, whereas, in my Before Times, pressure focused my thinking quite well.
A point of pressure I brought up was that I am really hating to be so useless. We came up with this: Andrew, 🤓 bring all the dry laundry up here and dump it on the bed!
Folding laundry is something I can still do! HA! I win!
I asked some other questions, but I’ll save those for a later round-up of Useful Info I collected this week from podcasts, studies, and TWIV.
He also mentioned that Long-COVID generally starts to show itself around the three-month mark after infection and gets progressively worse for +/- six months. We’re hoping this means I’m roughly at or nearing the nadir of this whole adventure.
I think this was his way of saying “you don’t yet know how many spoons you have, so figure that out first.” Ah, Spoons…kind of like this about using Elephants as a unit of measure.
“Tiny bits” means take your baseline of safe activity, then take what you think you can add to that day to stretch yourself—then cut that in half. “Today I think I could go for a walk in the morning (baseline) AND record the week’s podcast episode (the addition)” — but in reality, plan to go for your morning walk, set up the files for recording, and stop there. The recording shall be completed the following day.
Quoth the Neurologist.
Though far less ‘explosive’ these days, thank G-d.
I am not making this up. I am also starting to think we should lobby for a name change. Instead of Long-COVID—which sounds kind of squishy and easy to ignore—it should be Post-COVID Dysregulation Syndrome (PCDS isn’t a horrible acronym, after all).
I think, however, it might just be that viral infections mess with B-12 in general—and COVID is very good at being a virus. 😒
I’m finding that my problems with word/memory recall is far less upsetting/problematic when I write for myself or here. If I’m having to write a text or email, I’m a wreck.
I think part of that is due to the decades-long habit I taught my former students: when in the Writing Zone, if you hit a word that you know is not the right one, type XXXX and come back to it later. Since I’ve been doing that forever, I don’t panic.
This is NOT true when speaking. Losing words—and worse, not being able to count on short-term or recent memory recall—absolutely wallops me with anxiety and depression.
Yes, a darning needle. It’s thicker than a flue-shot needle but smaller than an ice pick. If I’d wanted to be really titchy I could have said “milliner’s needle” but that seemed too much even for me.
Basically, treat me like a 2-year-old…but with an adult tone-of-voice. 😜





Hi Heather, Sonya Lee here aka “ChickieLou”. I’ve been so hesitant to weigh in because while I do not have LC, have never even had COVID (yet), I’ve been experiencing repercussions from the vaccine and if you knew me, you’d know the absolute near-shame I feel in texting those words. I am absolutely pro science and pro vax. But here I am with an ever worsening heart arrhythmia obtained (lucky me) after the last vaccine, on the very night of the vaccine October 12 until last night. The cardiologist put me through every test, deemed it benign (my Apple Watch was saying A-Fib) and rather than reassuring me and contributing less stress, it grew steadily worse over time until I was looking at anti-arrhythmia drugs. (Do not want!)
Anyway, I have been wanting to tell you, while you are going through your labs and work up for this, be sure to ask about getting your Vitamin D checked. At my last physical in August, we almost dismissed this test because I walk 3 miles every day in the high desert of central Oregon (listening to podcasts!) My skin is not particularly tanned (which resists D uptake). So doctor and I assumed it would be normal but “let’s do it anyway”. Well! It came back very very low. So low, it’s dangerous! She put me on a pharmaceutical grade Vitamin D (50000 IU weekly for 8 weeks). I’m 4 weeks into the therapy. And while I can’t say my arrhythmia is gone, it has improved. My chronic fatigue and brain fog, as you can imagine with this deficiency, is profoundly better. Anyway, I thought today was the day to share that, in case your doctors feel testing this wouldn’t hurt. I’m sort of evangelizing about it now to all my friends and family (who were absolutely shocked that this could happen to me who practically lives outdoors.) I’m hoping to be able to get my booster in December.
Love you Heather and wish you nothing but good health.